Most rebreather divers start off their diving career with open-circuit diving; that is, with scuba. And some of them pick up bad habits. I happen to be one of those divers.
With scuba you start the dive with a very limited amount of air in your scuba bottle. New divers are typically anxious, breathe harder than they have to, and blow through their air supply fairly quickly. More experienced divers are relaxed and enjoy the dive without anxiety, and thus their air bottles last longer than they do with novice divers.
So early in a diver’s experience he comes to associate air conservation with a sign of diver experience and maturity. When you are relaxed and physically fit, and your swimming is efficient, your breathing may become extraordinarily slow. Some call it skip breathing — holding your breath between inhalations.
I was once swimming among the ruins of Herod’s Port in Caesarea, and my dive buddy was a Navy SEAL.  I started the dive under-weighted, so I picked up a 2000 year old piece of rubble and carried it around with me as ballast. In spite of the very inefficient style of swimming which resulted, my air supply still lasted longer than that of my SEAL buddy.
I started the dive under-weighted, so I picked up a 2000 year old piece of rubble and carried it around with me as ballast. In spite of the very inefficient style of swimming which resulted, my air supply still lasted longer than that of my SEAL buddy.
At first I was annoyed that I had to end the dive prematurely, but then I began to feel somewhat smug. I had used less air than a frogman.
As a physiologist I knew that I may well have been unconsciously skip breathing, which would have raised my arterial carbon dioxide level, potentially to a dangerous level. But all ended well, and I could not help being glad that I was not the one to call the dive.
It is important for rebreather divers to understand that they don’t have to be breathing elevated levels of carbon dioxide to run into physiological problems with carbon dioxide. It’s the carbon dioxide in your arterial blood that matters. It can render you unconscious even when you’re breathing gas with no carbon dioxide at all.

Normally the body automatically ensures that as you work harder, and produce more carbon dioxide in your blood stream, that you breathe more, forcing that CO2 out of your blood, into the lungs, and out through your mouth. It works like an air conditioner thermostat; the hotter it gets in the house, the more heat is pumped outside. In other words, arterial and alveolar CO2 levels are controlled by automatic changes in ventilation (breathing.) In fact you can predict alveolar levels of CO2 by taking the rate at which CO2 is being produced by the body and dividing it by the ventilation rate. This relationship is called the Alveolar Ventilation Equation, or in clinical circles, the PCO2 Equation.
Normally, CO2 production and ventilation is tightly controlled so that normal alveolar and arterial CO2 is about 40 mmHg, mmHg being a unit of so-called partial pressure. 40 mmHg of arterial CO2 is safe. [One standard atmosphere of pressure is 760 mmHg, so ignoring the partial pressure of water vapor and other gases, a partial pressure of 40 mmHg of CO2 is equivalent to exhaling about 5% carbon dioxide.]

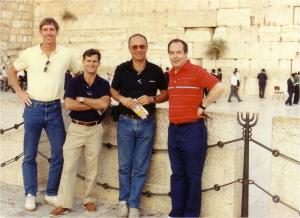
As an example, I once had as an experimental subject a physically fit Navy diver at the Naval Medical Research Institute during a study of respiratory loading. The test was conducted in a dry hyperbaric chamber under the same pressure as that at 300 feet of sea water. The experimental setup in the chamber looked somewhat like that in the figure to the right although the diver I’m talking about is not in this photo.
The diver was exercising on the bicycle ergometer while breathing through a controlled respiratory resistance at 300 feet in a helium atmosphere. The diver quickly learned that by double breathing, starting an inspiration, stopping it, then restarting, he could confuse the circuitry controlling the test equipment, thus eliminating the high respiratory loading.
As he played these breathing pattern games my technician was monitoring a mass spectrometer which was telling us how high his expired CO2 concentration was going. The exhaled CO2 started creeping up, and I warned him that he needed to cut out the tricky breathing or I’d have to abort the run.
The clever but manipulative diver would obey my command for a minute or so, and then go back to his erratic breathing. He joked about how he was tricking the experiment and how he felt fine in spite of the high CO2 readings.
That was a mistake.
When you’re talking, you’re not breathing. Since his breathing was already marginal, his end-tidal CO2, an estimate of alveolar CO2, shot up in a matter of seconds from 60 to 70 and then 90 mmHg, over twice what it should have been. When my technician told me the diver’s exhaled CO2 was at 90 mmHg, I yelled “Abort the run”. But the diver never heard that command. He was already unconscious and falling off the bike on his way to the hard metal decking inside the hyperbaric chamber.
The diver thought he was tricking the experiment, but in fact he was tricking himself. Although he felt comfortable skip breathing, he was rapidly pedaling towards a hard lesson in the toxicity of carbon dioxide.
Keep in mind, this diver was breathing virtually no carbon dioxide. His body was producing it because of his high work level, and he was simply not breathing enough to remove it from his body.
In upcoming posts we’ll look at what happens when inspired CO2 starts to rise, for instance due to the failure of a carbon dioxide scrubber canister in a rebreather. I already gave you one example in the CO2 rebreathing study of my first post in this series. There’s lots more to come.